The American Nurses Association (ANA) scored several legislative wins with the enactment of the latest funding package.
On February 3, President Donald Trump signed the Consolidated Appropriations Act, 2026 (Public Law No. 119-75) into law to end the partial government shutdown.
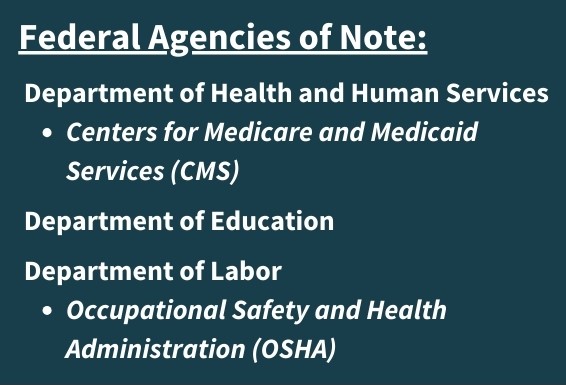
This $1.2 trillion package funds most of the federal government, including the U.S. Department of Health and Human Services, through September 30, 2026. The measure separately provides a continuing resolution that funds the U.S. Department of Homeland Security (DHS) for two weeks to give lawmakers extra time to negotiate a longer-term DHS bill.

The law provides funding for or extends several healthcare programs that are critical to nurses and the patients they serve:
- Title VIII Nursing Workforce Development Programs
- National Institute of Nursing Research (NINR)
- Telehealth flexibilities
- Dr. Lorna Breen Health Care Provider Protection Reauthorization Act
- PREEMIE Reauthorization Act
- Preventing Maternal Deaths Reauthorization Act
- Medicaid
Here is a glimpse of several legislative wins for ANA and the broader nursing community for fiscal year (FY) 2026 in this package:
Continued Funding for Critical Nursing Programs and NINR
Public Law No. 119-75 provides static funding – $305.472 million – to the Title VIII Nursing Workforce Development Programs in FY 2026. For those new nursing policy wonks, the Title VIII Programs are administered by the Health Resources and Services Administration and address all aspects of nursing workforce development, including education, practice, and retention.
While static funding may not sound like progress, it was a HUGE win given that a previous version of the Labor-HHS-Education spending bill in the U.S. House of Representatives would have cut roughly $47 million from Title VIII by eliminating funding for the Nurse Faculty Loan Program and the Nursing Workforce Diversity Program. ANA and 64 additional organizations comprising the Nursing Community Coalition worked tirelessly to express the nursing community’s concerns with the proposed cuts. Ultimately, the final measure provided level funding by simply reallocating $2 million from the Nursing Workforce Diversity Program to other programs within Title VIII.
The law also provides $197.693 million for the National Institute of Nursing Research (NINR) and $19.5 million for the Substance Abuse and Mental Health Services Administration (SAHMSA) Minority Fellowship Program (MFP). Within the National Institutes of Health, NINR conducts and invests in nursing research and training. The SAMHSA MFP aims to improve behavioral health outcomes for all by providing professional development and training opportunities for nurses and other healthcare professionals who comprise the behavioral health workforce. ANA is a proud MFP grantee organization. The static funding that NINR and the MFP received is a huge feat for ANA and its coalition allies given that the President’s FY2026 budget called for the elimination of NINR and reorganization of SAMHSA into the proposed Administration for a Health America (AHA).
Extension of COVID Era Telehealth Flexibilities
Public Law No. 119-75 extends telehealth flexibilities that were first put into place during the COVID-19 public health emergency through December 31, 2027. This extension prevents a sudden return to pre-pandemic requirements and ensures patients’ access to healthcare services through telehealth. Specifically, these flexibilities allow beneficiaries to receive virtual care from their homes without geographic limits, let a broad array of clinicians furnish telehealth services, and continue coverage for audio-only visits and other remote care modalities that increase access to care.
Reauthorization of Critical Programs that Support Provider Wellbeing
The Dr. Lorna Breen Health Care Provider Protection Reauthorization Act (H.R. 929/S. 266) was enacted into law as part of the funding package. This measure reauthorizes, through FY2030, critical programs that aim to prevent suicide and reduce occupational burnout, mental health conditions, and substance disorders among nurses and other clinicians. Initiatives include evidence-based treatments, suicide and burnout prevention training, and national education and advocacy campaigns to improve awareness and reduce stigma around getting help. For the first time, grant eligibility will now be expanded to include entities focused on reducing administrative burdens on nurses and other clinicians.
ANA was proud to advocate for reauthorization of these programs in collaboration with the Dr. Lorna Breen Heroes’ Foundation and other healthcare organizations through the All In Wellbeing First for Healthcare Coalition.
Maternal & Child Health Funding and Reauthorizations
Public Law No. 119-75 includes FY 2026 funding for several maternal and child health programs, including Healthy Start, the Maternal and Child Health Services Block Grant, newborn screenings, the Safe Motherhood Initiative, and the Maternal Mental Health Hotline.
The package also reauthorizes critical maternal and infant health programs through the passage of the PREEMIE Reauthorization Act (S.1562/H.R. 1197) and the Preventing Maternal Deaths Reauthorization Act (S.2621)/H.R. 1909) through FY2030. These programs advance research, education, and interventions to reduce preterm birth, while bolstering federal support for maternal mortality review committees that help states better understand and prevent pregnancy-related deaths. ANA was proud to partner with 260+ partner organizations to advocate for the reauthorization of these programs.
Medicaid Makes a Comeback
Last year, ANA and its allies were crushed when Congress voted to overhaul the Medicaid program through the enactment of the One Big Beautiful Bill Act, despite our extensive advocacy efforts to defend the program. While the program is still slated to undergo significant changes that will impact patients’ access to care and the nursing workforce, the funding law enacts bipartisan measures that aim to improve access, coverage, and program administration.
The Accelerating Kids’ Access to Care Act of 2025 (H.R. 1509/S. 752) requires states to establish a process through which qualifying out-of-state providers can temporarily treat children under Medicaid and the Children’s Health Insurance program without undergoing additional screening. The Ensuring Access to Medicaid Buy-In Programs Act (H.R. 1598) removes age restrictions on Medicaid eligibility for working adults with disabilities, allowing them to maintain coverage beyond age 65. The funding package also requires states to adopt clearer residency and coverage standards for military families. Finally, Public Law No. 119-75 directs the states and HHS to study the costs of maternity, labor, and delivery services to help inform Medicaid payment policies in the future.