This year was a busy and turbulent time for all of us as we continued to navigate life under the COVID-19 pandemic—and nobody knows this more than nurses and healthcare workers. While nurses across the country continued to provide valuable care to their patients, the Policy and Government Affairs team at American Nurses Association focused 2022 on highlighting the value of the nurse in our health care delivery system.
So, what do we mean when we talk about the value of the nurse? This takes a multitude of forms under our legislative and regulatory advocacy. We urged lawmakers to look at workplace challenges faced by nurses such as safety and staffing, advocated for the removal of barriers to practice, and the need to increase reimbursements for nursing services—all to strengthen and bolster the future of the profession. In a tumultuous year, we advocated for nurses and made important progress that will carry us into the new legislative session in 2023.
Legislative Recap
A Successful Spring
In March, President Biden signed the Dr. Lorna Breen Health Care Provider Protection Act into law. This law will identify and disseminate best practices to reduce and prevent mental and behavioral health conditions, suicide, and burnout, as well as increase access to evidence-based treatment for nurses and other health care professionals. Over 7,500 nurses like yourself sent a letter to Congress urging them to pass this bill, and we want to thank you for your help getting this bill signed into law.
March proved to be a successful month for ANA, as there were some key pieces of legislation for nurses passed in the omnibus appropriations bill.
- Title VIII Nursing Workforce Development Programs received $280.472 million dollars. This is $16 million more than these programs received in 2021.
- The National Institute of Nursing Research received $180. 862 million. This is a nearly $6 million increase over the fiscal year enacted levels!
- The Sexual Assault Nurse Examiners Program received $13 million, which is an increase of $4 million dollars. This funding will directly impact the Advanced Education Nursing program to expand training and certification of RNs, APRNs, and Forensic Nurses to practice as sexual assault nurse examiners.
- Nursing also received nearly $5 million for Nurse Education, Practice, Quality and Retention efforts to address the RN shortage. The agreement directs Health Resources Service Administration (HRSA) to give priority in new funding announcements to public entities for training of additional RNs, specifically for acute care settings. In addition, it directs HRSA to give priority to applicants in States listed in the HRSA publication “Supply and Demand Projections of the Nursing Workforce 2014-2030” as having the greatest shortages.
An Auspicious Autumn
ANA has made meaningful progress on several vital pieces of legislation that we will continue to advocate for in 2023 and the 118th Congress.
This year, ANA worked with Congress on the Improving Access to Workers’ Compensation for Injured Federal Workers Act. This legislation would improve the Federal Employees Compensation Act and close a loophole negatively impacting Nurse Practitioners (NPs) and their ability to provide care to federal employees who are injured at work. This common-sense legislation passed in bipartisan fashion in the U.S. House, and in 2023 ANA will continue our work on this bill.
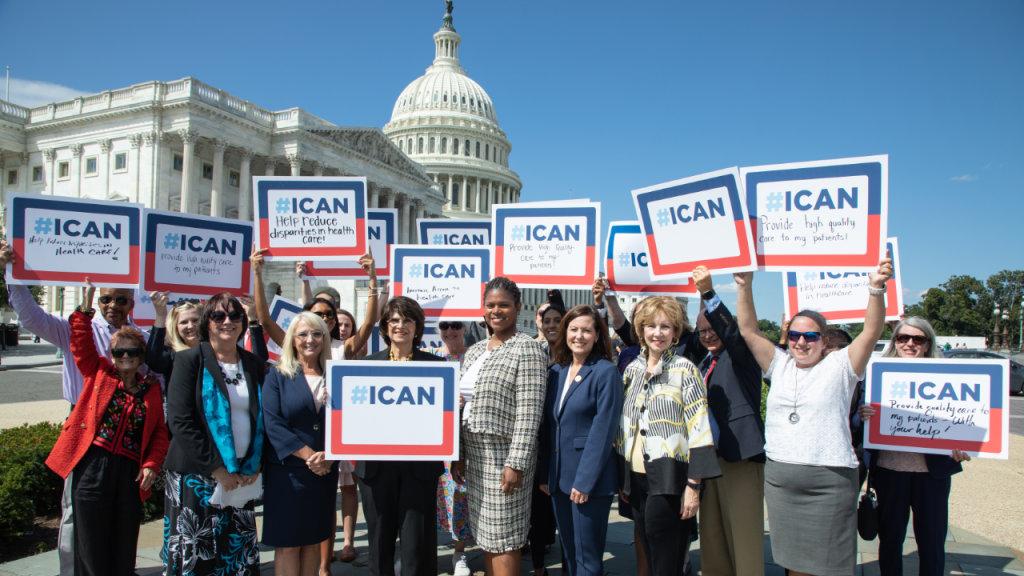
In September, ANA worked with several other nursing organizations and Congressional Representatives Lucille Roybal-Allard (D-CA) and Dave Joyce (R-OH) to introduce the Improving Care and Access to Nurses, or #ICAN Act, in the U.S. House. If enacted, this bill will remove practice barriers for advanced practice registered nurses (APRNs), improving access to care for Medicare and Medicaid patients. Read more about the #ICAN Act here.
In December, ANA worked closely with Senator Jeff Merkley (D-OR) to introduce the #ICAN Act in the Senate – a huge step forward to get the bill passed into law. Nearly 3,000 nurse advocates have written to their elected officials in support of this important legislation. You can join them, here.
Also in December, we continued our work with Senator Merkley, and worked with him to introduce the Nurse Overtime and Patient Safety Act in the U.S. Senate. As you know, many nurses have been forced to work overtime to alleviate staffing shortages. Substantial use of mandatory overtime can jeopardize patient safety and nurse well-being. A recent ANA survey found that nearly 60% of nurses reported being required to work beyond their shift on a weekly or even daily basis. This is unacceptably high, and Congress must rectify the issue. The trucking and aviation industries have federal mandatory overtime protections—nursing and health care are long overdue for the same safeguards. Learn more and email your senators, here.
Regulatory Recap:
A Strong Summer
Every year, CMS issues proposed rules related to Medicare reimbursement for services provided to patients. ANA uses this opportunity to comment on provisions that impact the nursing profession, highlight staffing and workforce challenges, and continue the drumbeat of the value of the nurse.
CMS also issued Requests for Information (RFI) throughout the year, allowing additional opportunities for ANA to share the nursing perspective on several topics. We weighed in on the impact of COVID-19, workforce challenges, rural health and health equity—all top priorities for ANA. In our comments, ANA asked CMS to remove barriers to practice, urged the agency to make the COVID-19 waivers permanent, and to continue to focus on workforce challenges and health equity. Read ANA’s comments, here, and learn more about our response to the Make Your Voice Heard RFI on the ANA Capitol Beat Blog.
In November, CMS released a memorandum on workplace violence in hospitals, reiterating that they will hold hospitals accountable for workplace safety. ANA is encouraged by this action, which signals that the administration is hearing our concerns around this critical issue.
A Winning Winter
In November, ANA’s Chief Nursing Officer, Debbie Hatmaker, and members of the Policy and Government Affairs team, met with Centers for Medicare and Medicaid Services (CMS) Administrator Chiquita Brooks-LaSure to discuss nurse staffing concerns, workplace environment and retention challenges, and the value of the nurse in today’s health care delivery system.
ANA staff also met with Center for Medicaid and CHIP Services Director and Deputy Administrator Daniel Tsai to discuss the Medicaid program once the COVID-19 PHE ends. We also discussed Director Tsai’s greater vision for the program as they work closely with states to expand coverage and access.
Rounding out the year, ANA staff attended a Department of Health and Human Services (HHS) event focused on maternal health and mortality. This event showcased the agency’s plan to tackle this important, pressing issue. ANA staff used this opportunity to articulate to agency staff the important role nurses play in addressing maternal health and the need for nurses to be included in any agency-led approaches.


ANA staff will continue its dialogue with HHS, CMS, and other subagencies in the New Year to ensure the nursing perspective is not only heard but incorporated. We also will continue to seek opportunities for engagement as our regulatory advocacy focuses on advancing the value of the nurse.
The Policy and Government Affairs Team is excited about the progress made legislatively and implemented through regulation in 2022 but we know our work on behalf of nurses and the nursing profession is never done. We look forward to 2023 and new opportunities to advocate for nurses and advance the nursing profession. ANA knows the value of the nurse, but we will make sure Washington does, too.


