This Capitol Beat article was guest-written by Debbi Waters, MSN, RN, MJ, CHC, a student in the McKendree University Doctor of Nursing Practice (DNP) in Ethical Leadership Program, who is completing her leadership practicum in partnership with ANA Senior Policy Advisor Lisa Stand.
This month, Congress took a positive step in preventing a repeat of the catastrophic shortages of personal protective equipment (PPE) experienced by nurses at the outset of the COVID-19 pandemic. With bipartisan support, the House of Representatives passed H.R. 3635, the Strengthening America’s Strategic National Stockpile Act of 2021.
It has been nearly two years since the COVID-19 pandemic began to rapidly spread across the United States (U.S.), triggering the worst public health emergency the nation has witnessed in more than a century. From the beginning of the pandemic in 2020, nurses quickly found themselves fearing for their personal safety, as well as the safety of their patients and families, as PPE supplies were being depleted at an extraordinarily fast pace. Nurses on the frontlines were directed to abandon evidence-based infection prevention standards, for instance, by being required to wear the same PPE for extended periods of time, and to reuse PPE across multiple shifts. In an American Nurses Association (ANA) survey in May of 2020, 45 percent of nurses reported experiencing PPE shortages, with 79 percent of nurses reporting being encouraged or required to reuse PPE, of those 59 percent felt unsafe in doing so. The ANA completed a second survey, ending on August 14, 2020, with 47 percent of nurses reporting intermittent to occasional PPE shortages. Forty-two percent of participating nurses reported an increase in PPE availability, as compared to 36 percent reporting no change; however, 68 percent continued to report being required by their facility to reuse single-use PPE, with 62 percent reporting feeling somewhat to very unsafe. The enormity of the impact of COVID-19 on healthcare workers is yet to be determined; however, the failure to provide basic PPE to frontline nurses and healthcare workers was profound and consequential to physical and mental well-being of our nation’s nursing workforce.
Why is H.R. 3635 Important?
H.R. 3635 would address key vulnerabilities within the federal government’s ability to adequately respond to such large-scale public health emergency, particularly with the medical supply chain.
The U.S., as with most other countries around the globe, utilized unprecedented amounts of PPE during the COVID-19 pandemic. At times, the PPE burn rate was nearly a 100 percent increase over historical levels. Very early in the pandemic as hospitals exhausted PPE supplies and began experiencing challenges in purchasing supplies through the usual “just in time” supply chain channels, and as local and state supplies became depleted, states called up the federal government for assistance through the Strategic National Stockpile (SNS)
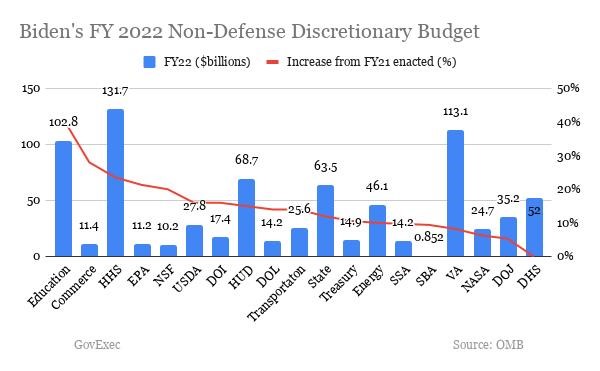
The SNS, long considered to be the contingency plan for public health emergencies, was ill-prepared to respond to a threat the size and scope of this pandemic, certainly not for a threat simultaneously affecting all 56 states, territories, and the District of Columbia. The SNS endured years of underfunding and budget cuts by Congress that, compounded by a failure to replenish and rotate stock, led not only to inadequate amounts of PPE, but also to the delivery of PPE that was expired, rotting, and inappropriate for safe use in protecting nurses from the dangers of COVID-19.
Maintaining the Stockpile
H.R. 3635 would address the issue of expired and unsafe supplies by allowing the U.S. Department of Health and Human Services (HHS) to distribute supplies from the SNS to any federal department or agency, on a reimbursable basis, if the supplies are within one year of expiration and can be replenished within the SNS. In addition, HHS would be required to ensure that supplies and equipment within the SNS are in working order.
Domestic Production
The COVID-19 pandemic also exposed the risks associated with U.S. dependence on foreign sources for nearly 60 percent of the nation’s medical supplies. This dependence created cataclysmic sourcing and price challenges for American hospitals and healthcare providers, caused by stockpiling of supplies and price gouging, at one point upwards of 1,000 percent the customary cost, for supplies that were of poor quality and at times counterfeit. The inability of domestic manufacturing proved to be detrimental to nurses who were providing care to COVID-19 patients. H.R. 3635 calls for the creation of a pilot program designed to strengthen the U.S. supply chain by increasing domestic manufacturing. Specifically, the pilot requires HHS to establish and maintain geographically dispersed domestic reserves of critical medical supplies, including PPE, and increased emergency stock of those critical supplies through cooperative agreements or partnerships with manufacturers to produce and maintain supplies. Additionally, the bill provides temporary authorization for HHS to disperse grants to states for use in maintaining or expanding state strategic stockpiles of critical supplies that are deemed essential by the State in preparation for future public health emergencies.
Transparency and Tracking
Strengthening America’s Strategic National Stockpile Act of 2021 would require HHS to develop a transparent process for distribution and use of supplies from the SNS by January 1, 2022. This would include a process for states, localities, tribes, and territories (SLTT) to request supplies; the decision-making process HHS will follow when determining if the request will be fulfilled or denied; and the process for the prioritization of distribution to the SLTT. In addition, the bill would require a monthly report to be provided detailing the requests submitted by SLTT, including the amount of materials and supplies requested, along with the outcomes of those requests. In the event a supply request is only partially filled or denied, the rationale for those outcomes must be included.
Our nation must begin building upon the lessons learned during the COVID-19 pandemic by planning and preparing a response to future public health emergencies. We must remain vigilant, as COVID-19 will not be an isolated incident, if we are going to prevent a repeat of the catastrophic failures experienced during the COVID-19 response. H.R. 3635 is a positive step towards ensuring the U.S. response to upcoming public health emergencies will be more efficient and effective, while protecting the health and safety of our frontline healthcare workers and we thank Representative Elissa Slotkin for her leadership in addressing this critical issue.
Next Steps
There is still work to be done to ensure the Strengthening America’s Strategic National Stockpile Act of 2021 is signed into law. This legislation now moves to the Senate where a companion bill S.1974 was introduced in June 2021. As you know, things tend to move slowly in the Senate and they need a groundswell of support from their constituents to pass legislation. Without action, nurses will be no more protected in future pandemics, than we were in March of 2020. Please visit our Latest News page for updates on the legislation and a chance for every nurse and health care advocate to take action and message their members of Congress soon.