As a result of effective advocacy by nurses, federal policymakers are gradually moving the needle to expand access to advanced practice registered nurses (APRNs). As so often is the case, added opportunities for APRNs can some with more oversight or potentially greater scrutiny. A case in point is Open Payments, which will shed sunlight on APRN relationships with drug and device manufacturers, due to upcoming implementation of a provision in the federal opioid response.
It has been two years since passage of the landmark legislation, the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act, or the SUPPORT Act. The SUPPORT Act unequivocally recognized APRNs as a key part of the nation’s response to the opioid epidemic. Specifically, Congress permanently enabled nurse practitioners (NPs) to obtain the necessary waiver to prescribe buprenorphine as treatment for opioid use disorders (OUDs). For certified nurse-midwives, clinical nurse specialists, and certified registered nurse anesthetists, this same authority is provided with a five-year sunset, ending in 2023. ANA is not done working with Congress to get permanent authority of all APRNs to prescribe Medication-Assisted Treatment (MAT).
Congress first expanded APRN authority to treat OUDs, on a temporary basis, in the Comprehensive Addiction and Recovery Act of 2016 (CARA). Elevating APRNs in the opioid crisis response has given patients with OUDs increased access to MAT. Medication-Assisted Therapy is a widely endorsed, evidence-based approach combining buprenorphine use with counseling and behavioral therapy. Allowing APRNs to prescribe buprenorphine has been especially beneficial in areas of the country experiencing shortages of healthcare providers. According to one analysis of CARA, the number of NPs prescribing buprenorphine increased by 79 percent, and rural counties had a higher proportion of advanced practice prescribers, including NPs, compared to urban counties.
At the same time, the SUPPORT Act included a provision that expands Open Payments to include information about drug industry payments to APRNs. That provision is set to be implemented over the next two years.
The Open Payments program is not new. Open Payments comes under the Physician Payment Sunshine Act, which Congress enacted as part of the Affordable Care Act in 2010. Open Payments allows anyone on the internet to look up their physicians (or teaching hospital), and soon other qualified health care providers, and find out about money or gifts their providers have received from sources such as drug companies, device manufacturers, and research sponsors. Open Payments was created out of the desire for transparency in certain health industry transactions, and out of concern that patient care decisions might be influenced by money from outside interests.
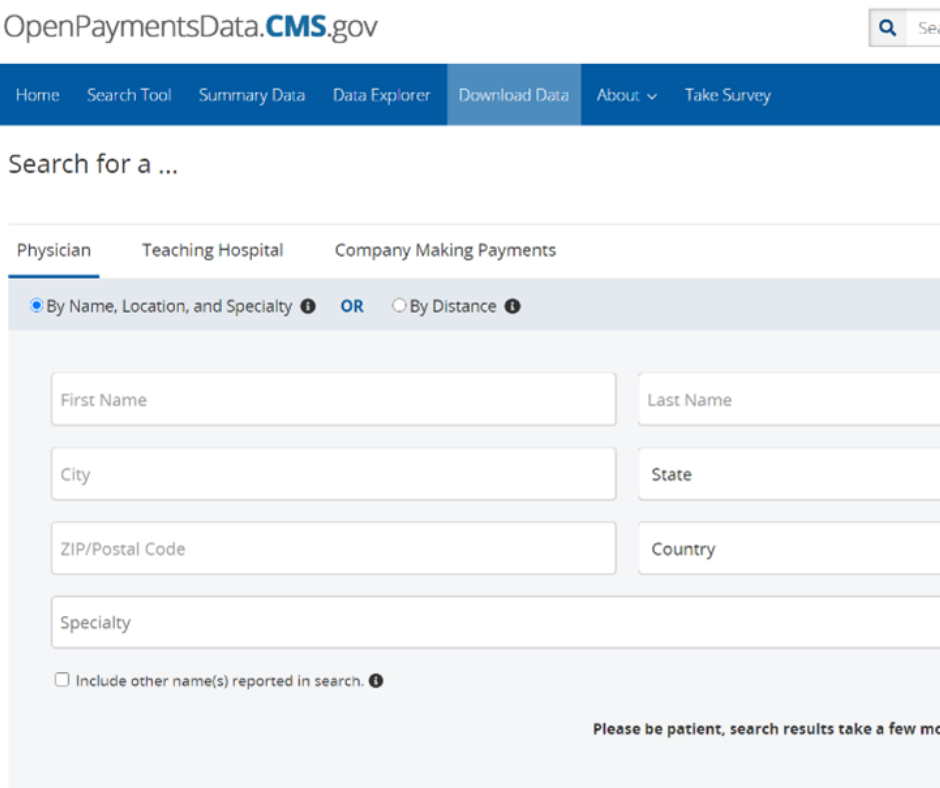
The Open Payments searchable database is maintained by the Centers for Medicare and Medicaid Services (CMS). As shown in the screenshot below, members of the public can visit the site and search providers by name and other information such as zip code.
A search reveals how much money a provider received in a given year, who made the payments, the types and nature of payment, and how receiving these payments compares to activity of other providers. The nature and types of payment include general payments, research-related payments, and food and beverage.
In addition to keeping and displaying the data, CMS conducts the process of collecting and vetting Open Payments information. Here’s how the process works, step by step:
- For each calendar year, manufacturers and other reporting entities transmit data on individual transactions (valued at around $11 or more) to CMS during an open reporting period in the following year, no later than March 31.
- After manufacturers and other entities report for the previous year, CMS prepares the data for disclosure to recipients identified by reporters.
- Recipients then have a window of time each Spring to review and verify information about them and ask for corrections if appropriate.
- Information for the previous year goes live on the Open Payments website each June.
For APRNs, step 3 will be important in 2022 and beyond, to ensure that reports of payments in the previous year are accurate. However, there are key steps that can be taken in 2021 to prepare. First, visit OpenPayments. Get to know the database and learn more about how to participate in the program. On the Open Payments site, there is a section titled Program Expansion and Newly Covered Recipients. Providers can also sign up for information and notifications.
To summarize, payments in 2021 from manufacturers to APRNs will be subject to reporting. In early 2022, the information will be entered in Open Payments. Affected providers will have a limited opportunity to review what is reported about them. The database will be updated with 2021 data in June 2022. This sequence will recur annually.