Advocating for a bill gets all the attention—thanks, Schoolhouse Rock—but the real action starts after a bill becomes law. Once the ink is dry, someone must figure out how that law will actually work in the real world.
That’s where regulation comes in.
Federal agencies take the laws passed by Congress, analyze them, interpret them, and translate them into detailed regulations—the practical roadmap for implementation. If a law is the diagnosis, regulation is the care plan.
Regulatory advocacy is your chance to shape that care plan. It’s the process of informing and influencing agencies as they develop, implement, and enforce the rules that bring laws to life.
And the best part: it’s one of the most direct, accessible ways to participate in public policy.
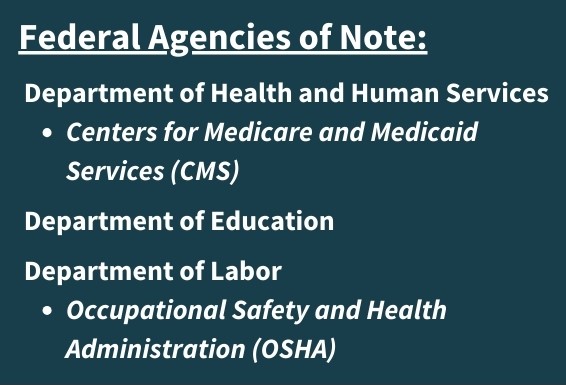
If you want proof that regulation matters, look at the Affordable Care Act. Congress passed a bill of a few hundred pages, but the real work—and thousands of pages of regulations—came from giving meaning to the 1,442 times the law directed “the Secretary of HHS” to implement the bill Congress had passed.
The Regulatory Cycle
Every agency has its own peculiarities when it comes to the process of issuing regulations, but the regulatory process follows a predictable rhythm. This article breaks down the key steps, shows you how to craft effective comments, and explains why nurses—because of their training, experience, and frontline perspective—are uniquely powerful regulatory advocates.
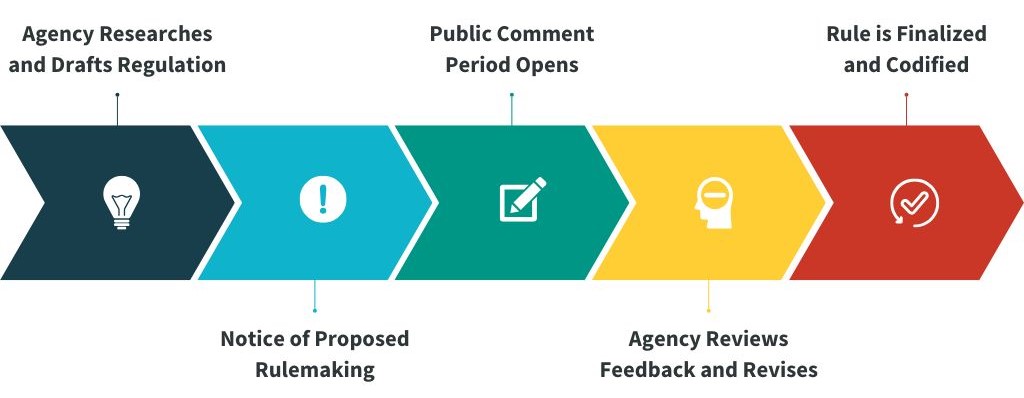
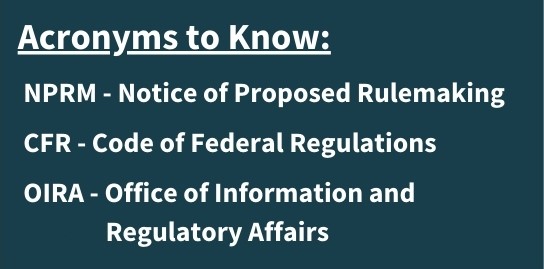
Once an agency finishes its research and drafts a regulation, it must alert the public through a Notice of Proposed Rulemaking (NPRM). The proposal, referred to as a proposed rule, is posted in the Federal Register, opening a public comment period. Comment periods vary from 30 to 60 days—where anyone can weigh in. After the comment window closes, the agency reviews the feedback, makes revisions, counts every comment and weighs the input to issue a final rule. That final rule is published in the Federal Register and added to the agency’s docket on Regulations.gov.
When a rule is finalized, it’s then codified in the Code of Federal Regulations (CFR)—the official, organized record of all federal regulations. The CFR is divided into 50 titles, each covering a major subject area. Most health care regulations live in Title 45, and the entire CFR is updated on a rolling annual schedule.
How to Track Regulations
If a rule is open for public comment, you’ll find it on Regulations.gov. That’s where you can submit your own comments and read what others have already posted (yes—every comment is public). If you want to follow an agency’s progress on a regulation, the Office of Information and Regulatory Affairs (OIRA) lets you track rules by agency and see where they are in the process.
Regulations can be long, but you don’t have to read every word.
Most NPRMs follow a predictable structure: instructions for submitting comments, a table of contents, background, a summary of the proposal, an analysis of its impact, technical details, and finally the actual regulatory text. If you want to see what’s changing, skip straight to the end.
Each notice also lists staff who can answer questions. They’re there for a reason—reach out.
How to Write a Regulatory Comment
Writing a regulatory comment is a lot like writing a SOAP note—you’re sharing who you are, what you see, and what you recommend, backed by real‑world experience and solid evidence. Comments can come from individuals or groups, and there’s no “right” length or format. What matters most is clarity, authenticity, and a strong point of view. Use this roadmap to craft an effective advocacy message:
Introduce yourself.
Briefly describe your professional background and relevant experience. Include credentials if you have them, and an email address if you choose. Skip anything confidential—no patient details or identifying information.
Be specific about what you’re responding to.
Name the exact section of the proposed rule you’re addressing and state your position clearly. Keep the issue front and center.
Use real‑world examples and impact.
Personal stories bring your perspective to life. They show how a policy affects people, workplaces, and systems—and making the emotional connect help connect with the reviewer.
Include evidence.
Data, citations, news articles and research strengthen your argument and show you’ve thought through the issue from multiple angles.
Offer or support solutions or alternatives.
Suggest solutions or highlight approaches that already work that the agency may have done. It is valuable to recognize the work being done as springboard to new regulation. You can also endorse ideas raised in other comments.
Educate.
Assume the reviewer has no clinical background. This is your chance to explain nursing practice and why your perspective matters.
Review before submitting.
Check for typos, clarity, and tone. Use professional language, spell out acronyms, and add subheadings if your comment is long.

